San Raffaele is the only center authorized to administer the medicine against ADA-SCID
After the positive opinion of the EMA, the European Commission approves the transfer of the marketing authorization for the gene therapy for the rare immunodeficiency ADA-SCID from the company Orchard Therapeutics to Fondazione Telethon. The drug is entirely the result of research by the San Raffaele-Telethon Institute for Gene Therapy (SR-TIGET) in Milan and the San Raffaele Hospital is the only center authorized for its administration
This is Fondazione Telethon's new challenge: for the first time in the world a non-profit organization will assume responsibility for the production and distribution of a medicine for a rare disease, gene therapy for the immunodeficiency ADA-SCID (Strimvelis).
Last year the Anglo-American pharmaceutical company Orchard Therapeutics PLC, owner of the product, announced its intention to disinvest in the field of primary immunodeficiencies. And today, after the positive opinion of the EMA, the European Medicines Agency, the European Commission approved the transfer of the marketing authorization in Europe for the same therapy to Telethon.
This medicine, for which AIFA authorized reimbursement in 2016, is administered at the San Raffaele Hospital in Milan, the only center authorized to date, and is entirely the result of research carried out by the San Raffaele-Telethon Institute for gene therapy (SR-TIGET) and the Telethon Foundation's commitment to transforming these results into a medicine. To date, a total of 45 patients have been treated at SR-TIGET, coming from over 20 countries around the world.

What is the ADA-SCID
ADA-SCID (adenosine deaminase deficiency severe combined immunodeficiency), also known as “bubble baby” disease, is a very rare, potentially fatal genetic disorder in which a defective gene blocks the production of an essential enzyme called adenosine deaminase (ADA), necessary for the production and maturation of lymphocytes, a particular type of white blood cell. Children born with ADA-SCID do not have a healthy immune system, so they cannot fight off the most common infections that can be fatal, and are forced to live in a sterile and isolated environment. The annual incidence is estimated between 1/375,000 and 1/660,000 live births [1]; based on data on newborns in the European Union (around 4 million per year), it is estimated that between 6 and 11 children are born with this pathology every year in the 27 EU countries.
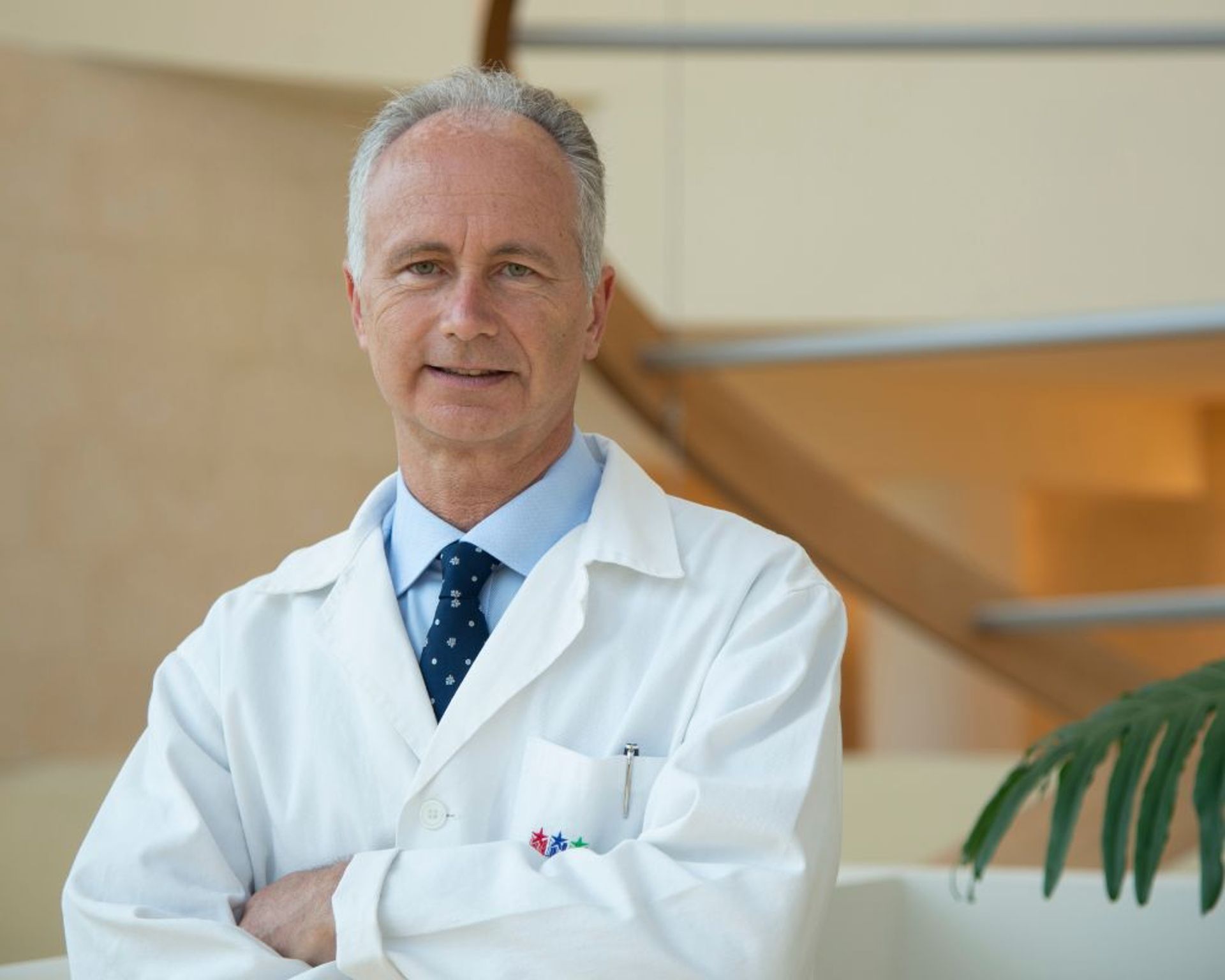
“The research that allowed us to develop this gene therapy began over 25 years ago. A result that is the fruit of the extraordinary work of the researchers and clinicians of the institute, as well as the support of the Telethon Foundation and all the donors.
In light of the benefits that we have seen in our young patients in recent years, who are now growing into adults, we can only rejoice in the fact that this gene therapy will continue to be available"
– declares Alessandro Aiuti, Professor of Peediatrics and deputy director and head of clinical research of the Institute.
A new model
“We are aware of the exceptional nature of this effort, but we cannot allow children with ADA-SCID to be left without this therapeutic option: we have decided to face this new challenge. It is a first step, but we would like it to become a model to be followed in other European contexts and to be extended to other drugs"
- explains the President of the Telethon Foundation Luca di Montezemolo.
“From this moment on, a paradigm shift will take place, because we can guarantee the availability of treatments that are not sufficiently profitable which would otherwise risk withdrawal or even lack of access to the market. We are the first non-profit organization to take on the marketing of a therapy: it is challenging, but we are convinced that it is the only way to remain faithful to ourselves and our mission"
- adds Francesca Pasinelli, General Director of Telethon.
How gene therapy for ADA-SCID works
Gene therapy for ADA-SCID is administered only once in a lifetime. The gene therapy drug is prepared from hematopoietic stem cells taken from the patients themselves, placed in contact with a vector of viral origin containing a corrected version of the defective gene in patients (ADA), which is able to restore the production of the missing protein due to the genetic defect. Reinfused into the blood, the corrected cells are able to differentiate even into the previously missing elements (lymphocytes), and thus defend the body from infections.

Therapeutic options
Today, there are several treatment options for ADA-SCID.
The first choice is represented by the transplant of hematopoietic stem cells from a compatible family donor, which can cure the disease but is available in less than 20% of cases [2].
When this type of therapy is not feasible, gene therapy represents a therapeutic option: it is based on a single administration of stem cells with the correct gene, which are taken from the patient's own bone marrow, significantly reducing possible transplant reactions against the host.
In the absence of these options, one can opt for a transplant from a compatible or partially compatible donor, with a potentially greater risk of incurring graft-versus-host reaction (GvHD), infections and other complications, even fatal in certain cases.
Finally, enzyme replacement therapy is available, i.e. the periodic intravenous administration of the missing enzyme produced artificially, which is generally administered for limited periods of time while waiting for a definitive treatment such as transplant or gene therapy [3].

[1] A. M. Flinn and A. R. Gennery, “Adenosine deaminase deficiency: A review,” Orphanet Journal of Rare Diseases, vol. 13, no. 1. BioMed Central Ltd., p. 65, 24-Apr-2018, doi: 10.1186/s13023-018-0807-5.
[2] J. Heimalla & M. Cowan, “Long term outcomes of severe combined immunodeficiency: therapy implications”. Expert Rev Clin Immunol. 2017 November ; 13(11): 1029–1040. doi:10.1080/1744666X.2017.1381558
[3] E. Grunenbaum et al, “Updated Management Guidelines for Adenosine Deaminase Deficiency”. J Allergy Clin Immunol Pract Vol 11, NUMBER 6. June 2023
You might be interested in

Multiple sclerosis, breakthrough in research: researchers have identified a molecule that promotes repair of the nervous system
The microbiome as an ally against myeloma

Intrecci: a UniSR project for more inclusive and accessible cancer diagnosis