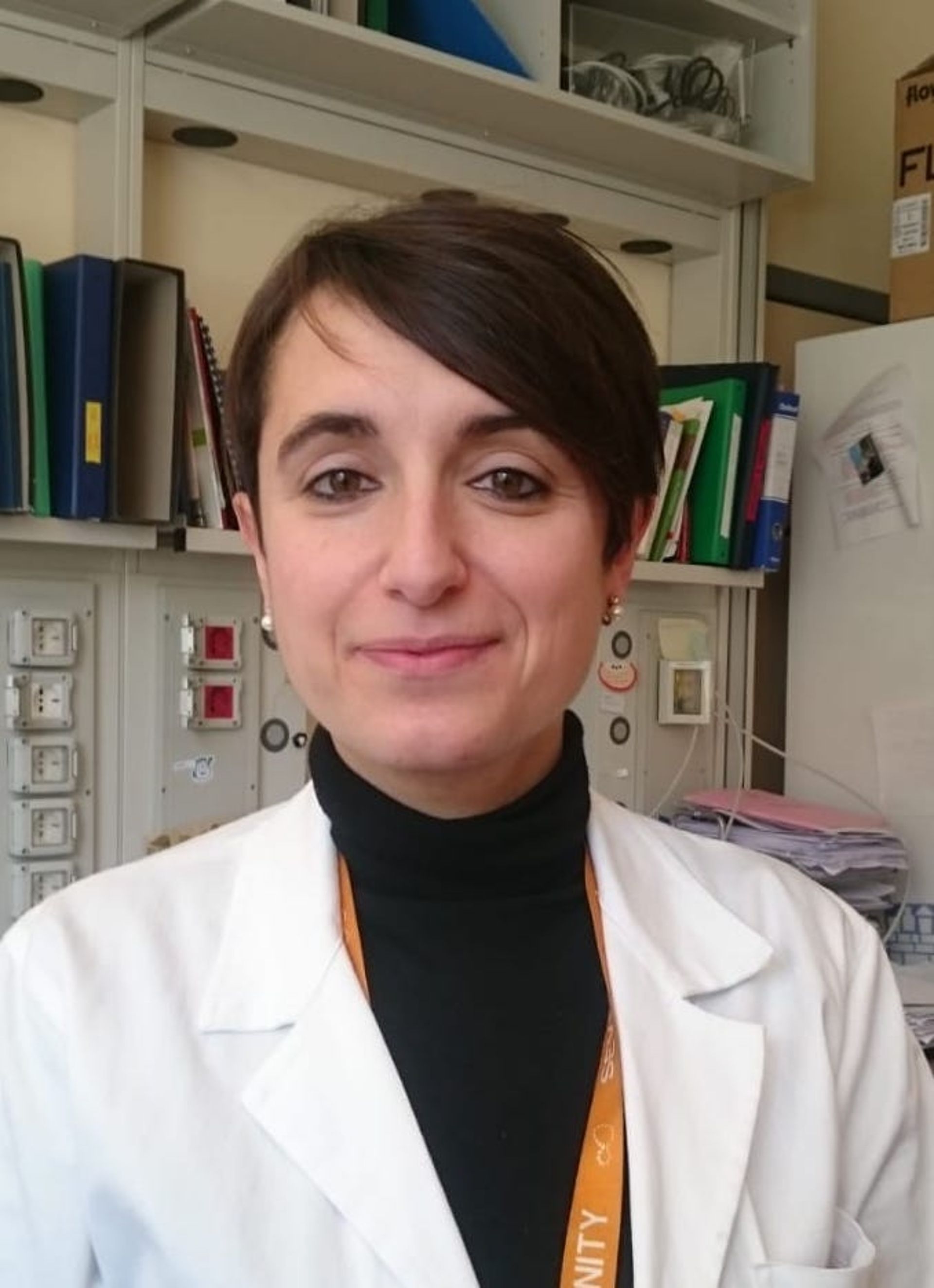
Antonella Antonelli is a young researcher in the field of leukemia immunobiology, concerned with understanding the biological phenomena that regulate the immune system's response against blood cancers. In particular, Antonella's team focuses on the study of acute myeloid leukemia; the primary treatment for this disease is transplantation, but unfortunately, up to a third of transplant patients experience a relapse that can have very serious consequences.
The goal of Antonella's research is to identify and characterize the molecular mechanisms underlying the post-transplantation relapses in these patients, with the aim of proposing new therapeutic strategies: for this project, she has won a Cariplo funding "Biomedical Research conducted by Young Researchers”, which offers researchers under 40 the opportunity to develop and enhance independent careers, conducting research projects under their own responsibility. "This funding came shortly after my return to research in Italy and after my maternity leave and gave me the motivational charge and financial support to get back into the game, to try to grow as a researcher and take the first steps towards my independence".
The transplantation problem in patients with Acute Myeloid Leukemia
"In the laboratory where I currently work, I mainly study acute myeloid leukemia in the context of allogeneic hematopoietic stem cell transplantation". Hematopoietic stem cells are the cells that will give rise to all the components of the blood: white blood cells, red blood cells, platelets. The allogeneic transplantation of these stems consists in their infusion by a healthy donor into a sick recipient, after the "conditioning" of the latter, i.e. the patient is prepared with the administration of high intensity chemotherapy and/or radiotherapy.
“Acute myeloid leukemia is a very aggressive, complex and heterogeneous tumor of the blood. Allogeneic transplantation is a procedure widely used today for patients with such disease; its effectiveness is based not only on the ability of chemotherapy and/or radiotherapy to eradicate the disease, but also on the immunological effect of the transplant itself, i.e the ability of the healthy donor T lymphocytes [a type of white blood cell, Editor's note] to eliminate the residual tumor cells possibly present in the recipient (an effect known as "Graft versus Leukemia"). Unfortunately, up to a third of these patients experience disease relapse after transplantation: in the absence of effective rescue therapies, post-transplantation relapses are the leading cause of death".

For the patients who relapse after transplantation, treatments such as the infusion of T lymphocytes from a healthy donor are currently suggested, to enhance the "Graft versus Leukemia" effect, or a second allogeneic transplant; unfortunately, in most cases they are not conclusive.
Recent studies [1],[2],[3] have shown how, following transplantation, leukemic cells develop mutations to "hide" and escape the newly transplanted immune system, which tries to destroy them: these genetic and epigenetic variations are the cause of relapse in patients. This phenomenon is called "leukemia immunoevasion". The laboratory of Dr. Luca Vago, Group Leader of the Unit of Immunogenetics, Genomics of Leukemias and Immunobiology, has been a pioneer in this field, describing in the last decade several molecular mechanisms which, as a whole, explain the development of relapse in about 60% of the patients analyzed. "Understanding these mechanisms in molecular detail is fundamental to propose new targeted immunotherapeutic strategies to combine with allogeneic transplantation to improve their long-term efficacy or to offer effective rescue therapies in the event of post-transplantation relapse".

Antonella's project
"Although the studies carried out on patient cells have been essential to demonstrate the importance of the phenomenon of immunoevasion in the development of post-transplant recurrences, the high variability among patients that characterizes these studies does not allow studying such mechanisms in molecular detail. To understand them it will therefore be essential to develop appropriate experimental models that effectively reproduce what happens in patients".
A skill, that in the generation of mouse models for the study of acute myeloid leukemia, which Antonella developed working for three years in Holland, and which she now applies in her work at San Raffaele.
"The mouse models called Patient-Derived Xenograft (PDX) allow recreating the conditions in the animal to study the complex interactions that occur between the donor's T lymphocytes and the patient's leukemic cells. In particular, in the project I coordinate will combine an advanced humanized mouse model of acute myeloid leukemia with the latest gene transfer techniques to screen genes and molecular processes potentially involved in the recognition of leukemia by donor lymphocytes".
Thanks to these studies it will be possible to improve the transplantations long-term efficacy by choosing the most appropriate rescue therapy, such as the use of immunotherapeutic drugs and targeted therapies able to enhance the anti-leukemic immune action, to overcome the evasion mechanisms put in place by leukemia.
[1] Zeiser and Vago (2019), Mechanisms of immune escape after allogeneic hematopoietic cell transplantation
[2] Toffalori et al (2019), Immune Signature Drives Leukemia Escape and Relapse After Hematopoietic Cell Transplantation
[3] Vago et al (2009), Loss of mismatched HLA in leukemia after stem-cell transplantation
Tags:
You might be interested in

A Francesco Andreata il Premio “Antonio Feltrinelli Giovani” per le Scienze Biologiche dell’Accademia Nazionale dei Lincei

UniSR takes the podium in Times Higher Education Rankings 2025

THE World University Rankings 2025: extraordinary results for UniSR