
"Epidemic", "pandemic", "contagion", "quarantine"...these are terms that in recent months we have come to know well, due to the COVID-19 emergency. Such concepts, however, are not at all unknown to mankind, which over the millennia has experienced a succession of epidemics, as pointed out by numerous historical evidences. What does History tell us, and what does it teach us? What lessons can we learn for the current situation? A concise but surely fascinating lesson in "History of epidemics" by Dr. Andrea Grignolio, History of Medicine teacher at the UniSR International Medical Doctor Program and Bioethics teacher at our Faculty of Medicine and Surgery.
Egypt, Rome, Constantinople: the first epidemics in History
Epidemics have existed since the first large urban gatherings existed. This is demonstrated, for example, by an Egyptian stele from the 18th dynasty (1403-1365 BC) where a scribe with a leg injured by polio is represented, or the mummy of the pharaoh Ramses (1157 BC), on whose face the pustules are still preserved of smallpox that probably killed him. Smallpox was in fact a disease capable of mowing down over 30% of the population, and which after millennia was eradicated from the globe in the late 70s of the last century, thanks to a worldwide vaccination campaign. The Antonine plague (165-80 AD) followed in Rome, caused by smallpox (or measles) which produced 30,000 deaths; always in Rome, a city that in ancient times reached the million inhabitants, a smallpox epidemic broke out with the Cyprian plague (in 250-270 AD), which at its peak counted 5000 deaths a day. The first bubonic plague, caused by the bacterium yersinia pestis, known as the "Justinian plague", raged from Constantinople to Rome between 541 and 750, killing 50% of the population, with an estimate that historians have calculated of about 30-50 million victims. Then there was a second wave of the same scourge 8 centuries later, the "black plague" narrated by Boccaccio, originating in Asia, which eliminated 30-50% of the population (30 million deaths).
Zoonosis, overpopulation, travels, wars: how an epidemic arises
A series of key elements contribute to the outbreak of an epidemic.
- Zoonosis, i.e. the jump of species from animals to humans that occurs in situations of close proximity to animals and poor sanitation. The domestication of plants and animals developed when, after the last ice age (12-10,000 years ago), men went from small groups of hunter-gatherers to permanent settlers. This change in habits favored the spillover process, the passage of viruses and bacteria to humans, whose immune system had to face these pathogenic parasites for the first time, unlike the animals that had learned to live with them for millennia thanks to a slow mechanism of coevolution and selection that had mitigated its virulence and pathogenicity.
- Population density. This element is one of the reasons that explains why the hunter-gatherer bands with groups of 30-50 individuals scattered throughout the Pleistocene period were free from epidemics, which on the contrary were frequent and fierce in the various urban settlements of the past.
- Commerce (for example the silk road was the vehicle of the medieval "black plague") and travels. As demonstrated by the origin of the "quarantine" in the ports controlled by Venice in the late 1300s and by many other historical studies, ports and ships (and today airport hubs) have always been a point of spread and multiplication of the infections. In the ships that in the early decades of the 1500s the Spanish conquistadores brought to South America not only weapons were present, but also infectious agents such as smallpox, measles, salmonella enterica of the paratyphoid type C or viral hemorrhagic fever. This explains how the 500 men of Cortés were able to annihilate the large Aztec army of Montezuma. It was a real hecatomb, if one thinks that the population of Mexico, then made up of about 25 million people, was reduced by 98% in just 100 years (22 million died, since in 1623 the inhabitants were now reduced 700,000 individuals).
- A last frequent element are therefore wars. Just think of the "Spanish" flu epidemic, which killed between 70 and 100 million individuals in the two years following the First World War.

Epidemics of the past, similarities with the present
Epidemics have often had the ability to shape the course of history. The first epidemic of historical importance was the Plague of Athens in 430 BC told by Thucydides during the Peloponnesian war, in which Sparta and Athens faced each other, and therefore two political models, oligarchy against democracy. In Athens under siege, the plague broke out, an epidemic (probably of typhus, or perhaps hemorrhagic fever) aggravated by poor sanitation due to promiscuity, food shortages and stress typical of conflicts. In this context of weakness of the Athenian army, the great strategist Pericles also died. The plague therefore favored Sparta and democracy vanished to reappear, although weakened, in some phases of republican Rome. Thucydides left us two basic teachings:
- those who get sick and survive are protected from the future encounter with the same disease (today we would say that they have "developed immune memory"), becoming useful figures for the care of the sick and the various social subsistence activities;
- among the groups that pay the highest price, there are doctors on the front line of epidemics.

History also teaches us the danger of irrational attitudes during epidemics: typical is the case of the search for a scapegoat, the “untore” (plague-spreader). During the terrible polio epidemic that spread in the United States in the early decades of the twentieth century, there was a social psychosis in search of the culprit, given the unclear origin of the disease. Accused were progressively moved to cats (60,000 were suppressed in New York in 1916), blueberries, Italian immigrants, milk and even sugar and ice cream, which were banned. In fact, it seemed that the number of polio cases increased during the heat (when eating ice cream was more frequent). This fact was also supported by research that suggested that the variation in sugar metabolism made it more sensitive to the disease – a lesson to keep in mind even today, both for the xenophobic accusations and for the daily acclamation of the media towards hypothetical miraculous cures.
Lessons for the current situation
History teaches us that epidemics, being based on mutual contagion, are democratic and therefore are to be fought together, sharing economic efforts, the same protective measures (individual safeguards and responsibilities, quarantine, etc. ) and certainly also international collaboration and data transparency. An example: in 1884 in Naples cholera had devastated the city, killing about 6 thousand people. In 1910 there was a second wave, described by Dr. H.D. Geddings, an American officer of the public health service in the port city, hub of migrations to America and center of "intelligence" in the Mediterranean of American health control. The local authorities and national policies, then under the Giolitti government, refused to recognize the existence of the outbreak claiming it was gastroenteritis, "Napolitan fever" or "Maltese fever" (the same accusation mechanism of the foreigner happened with the syphilis named "French disease" and "Spanish flu", which were neither attributable to the French nor the Spanish). Geddings was silenced and the epidemic was declared over after a month, although it continued to rage until the spring of the following year. That is why today with Covid-19 states should offer maximum collaboration on data, to limit unnecessary loss of lives and to show that the more you work together against viruses, the sooner you win.

Cover image: Nicolas Poussin, The Plague of Ashdod (1630), WikiCommons
Text images:
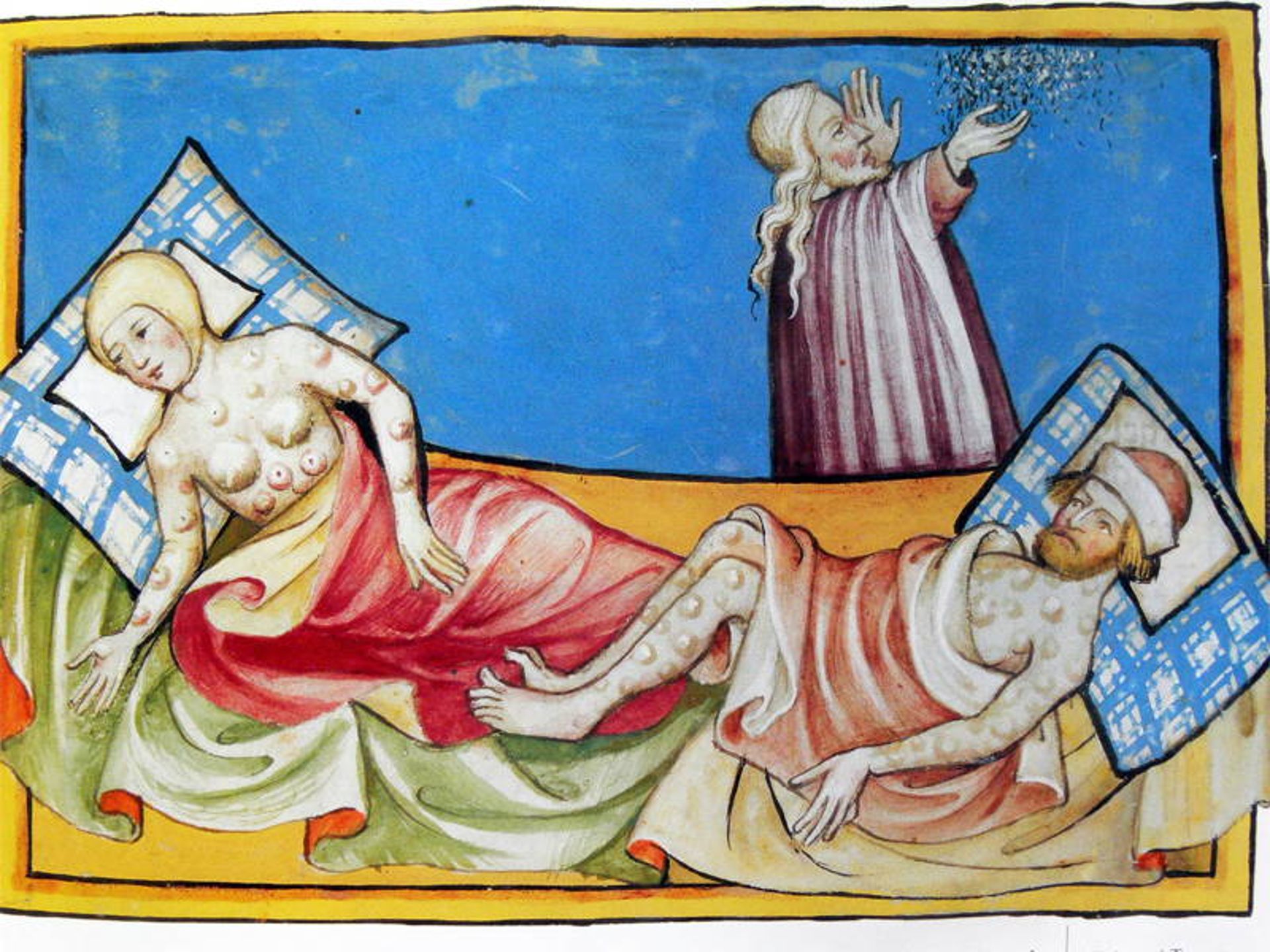
- The black plague disease (Miniature out of the Toggenburg Bible, Switzerland, 1411)
- ShutterStock
- Plague in an Ancient City, Michiel Sweerts (c. 1652–1654), WikiCommons
- "Malta: view of the quarantine area". Etching by M-A. Benoist, c. 1770, after J. Goupy, c. 1725
You might be interested in
/resolutions/res-c660x528/Pensa_Aorta_Congresso_UniSR-(3).png)
UniSR hosts the launch of the “Pensa all'Aorta” campaign

UniSR PhD Courses 2025-2026
0/resolutions/res-c660x528/Cassandra_studio_pazienti_pancreas_UniSR-(1)0.png)
Pancreatic Cancer: New Treatment Guidelines Arising from a Patient-Funded Study
/resolutions/res-c660x528/Milani_terapia_genica_UniSR-(1).png)
